Volume Control- Continuous Mandatory
Ventilation with a “Set-point” targeting scheme (VC-CMV(s)) is likely the most
utilized mode of mechanical ventilation in adult patients in North America.
This is due to a few a reasons:
1. VC-CMV is a standard mode on almost every
intensive care ventilator and anesthesia delivery system.
2. VC-CMV is one of the first modes of mechanical
ventilation.
3. VC-CMV is easy to understand in both theory
and operation.
4. VC-CMV is the standard of care when
ventilating patients with Acute Respiratory Distress Syndrome (ARDS) and Acute
Lung Injury (ALI).
5. VC-CMV is the standard of care for adult
patients intraoperatively.
The key advantage of VC-CMV(s) is the
safety and simplicity of the set-point targeting scheme. The operator can
manually set all parameters of the volume/flow waveform and adjust the minimum
minute ventilation parameters (relating to frequency and tidal volume). “One
can quickly trouble-shoot a patient’s situation, so during a change the
operator can diagnose the problem and intervene rapidly”. [1]
When one sees a mode of ventilation
labeled “Volume Control”, “VC”, “Volume A/C”, or “CMV” it affirms that the
breathing pattern delivered to the patient will consist of a constant tidal
volume and inspiratory flow waveform (fig.
1)
 |
| Figure 1. Volume Control Ventilation Breath Pattern. |
 |
| Figure 2. Volume and Flow waveform remains constant even-though compliance decreased to 25, compared to Figure 1. |
regardless of changes in a patient’s respiratory system mechanics and/or
inspiratory drive (fig. 2) [2]. Conversely,
due to no industry standard for ventilator mode taxonomy and medical device
manufacturers marketing schemes the actual breath delivered to the patient does
not resemble the predicted breath pattern and may result in a tidal volume much
larger than the expected preset value.
How does this happen?
EXAMPLE 1: DECEPTION
The device operator selects a mode
labeled “Volume Control” and the breath delivered actually resembles a Pressure
Control or Pressure Support breath. This is due to the modes “targeting scheme”.
A targeting scheme is the third building block for constructing a mode of
mechanical ventilation the first is “Ventilator Control Variable” and second is
the “Breath Sequence” [3]. The targeting scheme is usually a closed-looped
feedback control system (similar to “If then statements” in conditional
computer programming) which tries to achieve a specific ventilatory pattern. Thus
making the targeting scheme the culprit for the change in breath pattern.
Volsko and colleagues [2] demonstrated
this well when comparing differences in VC-CMV(s) and VC-CMV dual targeting
(VC-CMV(d)). The researchers used an ASL 5000 lung model (Ingmar Medical) and
simulated the pulmonary mechanics of an adult patient with ARDS during active
and passive ventilation. During the simulated spontaneous breathing VC-CMV(s)
delivered a consistent tidal volume similar to operator settings. However,
VC-CMV(d) delivered a breathing pattern similar to pressure support resulting
in higher flow rates and delivered tidal volume.
The deception is buried in the
manufactures naming of the mode. In this study researchers used the “Volume
Control” mode on the Servo-i ventilator for the dual targeting scheme arm of
the study. The name “Volume Control” and the generic settings (fig. 3) associated with the mode on the Servo-i misleads the operator to
believing that the mode is simply VC-CMV(s). The Dual Control targeting scheme
happens behind scenes in which the device operator cannot control.
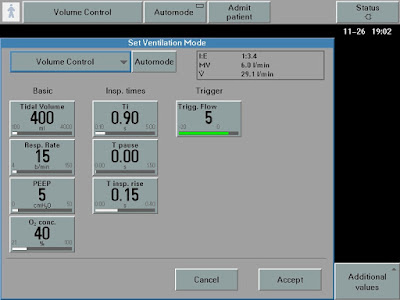 |
| Figure 3. Settings for Volume Control on the Servo-i ventilator. |
The mode mimics the standard set-point
functionality associated with the traditional VC-CMV(s), until the patient
makes an inspiratory effort that decreases the inspiratory pressure by 3 cmH2O.
If this happens “the ventilator switches to pressure control and, if the effort
last long enough, flow cycles the breath” similar to pressure support [4]. Thus
delivering a higher inspiratory flow resulting in a larger tidal volume than
predicted (fig. 4).
 |
| Figure 4. Screen shot demonstrating the dual control targeting scheme of Volume Control in the Servo-i, the inspiratory flow increases based on patient effort resulting in a higher tidal volume. |
EXAMPLE 2: ADJUNCTS
As mentioned in previous posts Adaptive
Pressure Control Ventilation (APC) may not provide consistent tidal volumes
during rapid changes in pulmonary mechanics and vigorous inspiratory efforts [5,6]. In
2007 Jaecklin demonstrated that APC in a variety of ventilators regularly
delivered excessive tidal volume in response to sudden increases in patient
compliance or decreases in resistance potentially putting neonates at risk for
lung injury [7].
Why do I mention APC? Isn’t it obvious that
APC is an entirely different mode then VC-CMV(s)?
APC actually classified as Pressure
Control-Continuous Mandatory Ventilation with an “Adaptive” targeting scheme or
PC-CMV(a) for short is much different than VC-CMV(s). The control variable,
breath sequence, and targeting scheme are unrelated, furthermore the names for some
of these modes “Pressure Regulated Volume Control (PRVC)” and “Adaptive
Pressure Ventilation (APV)” make it difficult for the operator to believe that
one of these modes is actually VC-CMV(s).
Unfortunately, the naming of a mode or
modality adjunct can confuse the operator making them believe the mode is
actually a volume controlled mode. I presented earlier how one may confuse
“Volume Control” on the Servo-i with VC-CMV(s) based on the name and how the
breath is delivered in a passive patient. Another example of this is in the
PB840 ventilator with a mode called “Volume Control Plus (VC+)” this mode in
fact is PC-CMV(a).
The mode adjunct “AutoFlow” on Draeger
Series ventilators may deceive likewise.
Some consider AutoFlow an individual
mode of ventilation, but I view it as an adjunct because it resides as an
option among the additional settings in volume targeted modes.
Figure five shows the traditional
settings for volume control ventilation on a Draeger V500 ventilator and figure
six displays the additional settings rooted in the VC-CMV(s).
 |
| Figure 5. VC-CMV settings on the Draeger V500. |
 |
| Figure 6. AutoFlow highlighted under additional settings of VC-CMV. |
From this page
the operator can turn on AutoFlow which switches VC-CMV(s) to PC-CMV(a). After
selecting AutoFlow the displayed mode name does not change the word AutoFlow is
added to it (e.g. VC-CMV, AutoFlow) (fig.
7).
 |
| Figure 7. Mode still labeled VC-CMV after AutoFlow activated. |
If the operator does not know that AutoFlow actually changes the mode
to PC-CMV(a) then they may assume that they are still in a volume control mode
and that a constant volume breath pattern will be delivered.
Volume Control-Continuous Mandatory
Ventilation with set-point targeting is a safe and simplistic mode of
ventilation that allows the operator to manually preset a minimum minute
ventilation and quickly trouble shoot during adverse events. Unfortunately, due
to no industry standards for ventilator mode taxonomy one can be misled using a
mode labeled “Volume control”, “Volume Control Plus”, or selecting a mode
adjunct expecting a volume control breath.
RELATED POST
Reference
1. Williams, K. et. al. (2011). Control
of Breathing During Mechanical Ventilation: Who is the Boss? Respiratory Care. 56 (2): 127-138.
2. Volsko, T. et. al. (2012). The
Effect of Targeting Scheme on Tidal Volume Delivery During Volume Control
Mechanical Ventilation. Respiratory Care.
57 (8): 1297-1304.
3. Chatburn, R. et. al. (2014). A
Taxonomy for Mechanical Ventilation: 10 Fundamental Maxims. Respiratory Care. 59 (11)
4. Chatburn, R. (2012). Standardized
Vocabulary for Mechanical Ventilation. Mandu Press Ltd.
5. APC: Variances in Delivered Tidal Volume.
6. Adaptive Pressure Control Ventilation:
Vigorous Inspiratory Drive.
7. Jaecklin, T. et. al. (2007). Pressure Control
Volume Targeted Modes of Modern Neonatal Ventilators: How Stable is the
Delivered Tidal Volume? Intensive Care
Medicine. 33 (2): 326-335.