Tuesday, January 8, 2013
Sunday, January 6, 2013
Simplifying Mechanical Ventilation
 |
| From Global Nerdy @ www.globalnerdy.com |
In a recent
letter to the editor “Ventilatory modes. What’s in a name?”[1] Authors provide
a strong argument for the need to standardize terminology in regards to
mechanical ventilation and propose an oversimplified classification system
specifically for non-invasive ventilatory devices. I applaud the authors for
their call to action; conversely their viewpoint is neither novel nor
applicable to ventilator taxonomy.
Friday, December 21, 2012
A Review of Plateau Pressure
What is Plateau Pressure?
Why is it important?
How can I measure plateau pressure?
In pressure control ventilation is the peak pressure and plateau pressure always equal?
Is plateau pressure always accurate?
Thursday, December 6, 2012
Tuesday, November 27, 2012
CPAP as a LOW TIDAL VOLUME VENTILATION STRATEGY
 |
| Image 1: Ventilator Screen Shot of Continuous Positive Airway Pressure. |
In October’s
issue of the Chest Journal, a few colleagues of mine authored the abstract “The Use of Invasive Continuous Airway Pressure for Low Tidal Volume Ventilation”.
This abstract was very intriguing to me for
various reasons, one this goes against many traditional methods of providing
ventilatory support for the patient with Acute Lung Injury and/ or ARDS.
Zealots of
Airway Pressure Release Ventilation would argue that using pure CPAP would lead
to extreme work of breathing and not off load the respiratory muscles
sufficiently.
I myself
would be concerned about using CPAP only, especially in extra-pulmonary ARDS primarily
sepsis and septic shock where patients metabolic demand is high, which leads to
a vigorous inspiratory demand. Off-loading these patients is very difficult and
even using APRV or traditional methods leads to severe hypercapnea.
However, I was baffled so I questioned my friend Troy Whitacre, a coauthor of the
abstract to find more details and to share his experience.
Labels:
Other
Monday, November 19, 2012
Video Games on the Brain
How Video Games may help us learn and focus.
Labels:
TED Talks
Tuesday, November 13, 2012
New Project: Concepts of Mechanical Ventilation
I have started a new project called "Concepts of Mechanical Ventilation".
This will be a educational page reviewing basic to advance concepts of mechanical ventilation.
I will be adding short educational videos, which links can be accessed under the "Video Library" tab at the top of this Blogs page.
The above video is an example, more to come.
Saturday, November 3, 2012
The Versatility of Mid-Frequency Ventilation
MFV first proposed in the medical literature in 2008 as a “conceptual”
[1] ventilator modality which maximizes alveolar ventilation and minimizes the
delivered tidal volume. MFV provides an alternative to traditional
Volume-Control (VC) ventilation for patients with ARDS. This is extremely beneficial because lung
protective strategies using VC ventilation are limited by predestined hypercapnia
and hypercapnic acidosis.
Sunday, October 21, 2012
Rebuttal to APC a False Sense of Security
 |
| Image 1: Laparoscopic surgery. |
After reading the post one could assume that I'm against using this mode of ventilation.
However, I believe this mode has many advantages.
Wednesday, October 17, 2012
Flu season not for me!: Surveillance screening for scheduling.
I have always believed in the motto "work smarter, not harder".
As a respiratory therapist one is paid hourly and it does not matter how much work you do in that hour. You will not receive a bonus if you administer 100 more breathing treatments then your coworker.
So what are the optimal times to be at work versus being on vacation, in regards to working smarter?
Monday, October 15, 2012
Publication Bias: Evidence Based Medicine Dirty Secret
Dr. Ben Goldacre presents the topic of research misconduct in medicine and how unreported negative trials may mislead practitioners to the actual safety of a pharmaceutical agent.
Goldacre, states that positive results are two times as likely to be published than the negative results and believes that all human trials should be published regardless of outcomes.
Labels:
TED Talks
Monday, October 1, 2012
Determinants and Limits of the Bellows: The Katz Study
 |
| Image 1: Draeger Narkomed 2c Anesthesia Delivery System. |
In a previous post "Determinants and Limits or the Draeger Narkomed Anesthesia Machine in Regards to Ventilating the Morbidly Obese Patient", I tried to calculate the largest patient a bellows system could ventilate safely.
I concluded that if you wanted to deliver a minute ventilation greater than 9 liters per minute, using conventional ventilator settings (tidal volume of 10 ml/kg/IDBW) that the operator would run into issues.
Labels:
Anesthesia
Monday, September 24, 2012
Designing Medical Equipment for the Real World
______________________________________________________
RELATED POST
Labels:
TED Talks
Monday, September 17, 2012
Adaptive Support Ventilation in the Morbidly Obese
Mechanically ventilating the morbidly obese patient has many considerations
Thursday, September 13, 2012
Dead Falls, Trip Wires, and Ventilator Settings
As many may
not know I grew up in the Midwest and was raised on the principles of self-reliance
and the respect for nature. I was taught how to hunt, fish, trap, forge,
and grow one’s own vegetables. Our family even attempted to save enough food
for a year, preparation for hard times or a catastrophic event (most likely a
tornado).
Labels:
Waveforms
Monday, September 3, 2012
Obtaining P0.1 on Various Ventilators
Airway Occlusion at 0.1 Second (P0.1)
In previous post I provide a brief description of the P0.1 and how one can apply this to adjusting settings on the ventilator [1,2] and provide greater detail in my book [3].
However, how does one obtain this measurement?
Fortunately, modern mechanical ventilators have this as a software option.
Even though the procedure for obtaining a P0.1 is automated, it is a little different on each device.
Sunday, August 26, 2012
Volume-Control to Pressure Control
 |
| Image 1: The Settings of VC-CMV. The settings highlighted in yellow are associated with patient-ventilator asynchrony. |
VC-CMV is likely the most utilized mode of mechanical ventilation. This is due to a few a reasons:
1. VC-CMV is a standard mode on almost every intensive care ventilator (table 1).
2. VC-CMV is one of the first modes of mechanical ventilation.
3. VC-CMV is easy to understand in both theory and operation.
4. VC-CMV is the standard of care when ventilating patients with Acute Respiratory Distress
Syndrome (ARDS) and Acute Lung Injury (ALI).
Labels:
Waveforms
Sunday, August 19, 2012
Frustrated with Medical Therapy Options? Design Your Own.
 |
| Image 1: Modeled Aorta. |
Labels:
TED Talks
Monday, August 13, 2012
Minimal Fresh Gas Flow: "A Reassuringly Safe Anesthetic Technique".
 |
| Image 1: Minimal FGF on the FLOW-i anesthesia delivery system |
In this months Canadian Journal of Anesthesia authors of the article "Brief Review: Theory and Practice of Minimal Fresh Gas Flow Anesthesia", conclude that with newer anesthesia delivery systems that using minimal fresh gas flow and third generation of inhaled anesthetic agents is a safe technique with many benefits [1].
The authors review advantages, potential limitations, and safety considerations when utilizing minimal fresh gas flow technique (mFGF).
Labels:
Anesthesia
Thursday, July 26, 2012
Setting PEEP
There is
many ways to set Positive End Expiratory Pressure (PEEP). Setting PEEP too low
may result in under or tidal recruitment of the lung and PEEP that is too high
results in over-distention, both contribute to Ventilator Induced Lung Injury
(VILI). This post provides a synopsis of
the various techniques as well as potential pros & cons.
Wednesday, July 18, 2012
Vent Graphics Contest WINNERS
First, I would like to thank all my readers who entered the "Vent Graphics Contest" , I appreciate all of the efforts.
First Prize
John Priest
Equipment Used: Epiphan
 |
| Image 1 & 2: Preventing auto-triggering. |
Labels:
Waveforms
Sunday, June 24, 2012
NAVA vs. Pressure Support in Pediatric Patients
 |
| Pressure Support Ventilation can be associated with 8 types of patient ventilator asynchronies. |
Overview
The
researchers sought to determine if neurally adjusted ventilatory assist (NAVA) enhances
asynchrony, ventilatory drive, breath-to-breath variability and COMFORT score
when compared to pressure support (PS).
Twelve pediatric patients with asynchrony (auto-triggering, double
triggering or non-triggered breaths) were enrolled in a non-randomized
short-term cross-over trial. Four
sequential 10-min periods of data were recorded after 20 min of
ventilatory stabilization (wash-out) at pre-determined settings.
Results
The
median asynchrony index was notably lower during NAVA than during 2-PS(opt) and
4-PS(opt). In NAVA mode, the NAVA trigger accounted for approximately 66% of
triggered breaths. The median trigger delay with respect to neural inspiratory
time was considerably lower during NAVA than during 2-PS(opt) and 4-PS(opt).
The median electrical activity of the diaphragm (EAdi) change during trigger
delay normalized to maximum inspiratory. EAdi difference was notably lower
during NAVA than during 2-PS(opt) and 4-PS(opt). Additionally, NAVA produced a significantly
higher coefficient of variation of tidal volume than 2-PS(opt) and 4-PS(opt).
The median comfort score during NAVA was lower than that during 2-PS(opt) and
4-PS(opt).
Conclusion
This
research shows that NAVA results in improved synchrony, reduced ventilatory
drive, increased breath-to-breath mechanical variability and improved patient
comfort compared to optimized PS.
Reference
De le Olivia, P., Schuffelmann, C., Gomez-Zamora, A., & Kacmarek, R. M., (2012). Asynchrony, neural drive, ventilatory variability and COMFORT: NAVA versus pressure support in pediatric patients. A non-randomized cross-over trial. Intensive Care Medicine, 38(5), 838-846.
Thursday, June 14, 2012
Capture the Flag: Vent Graphics Contest
http://www.youtube.com/user/devinsupertramp
I have many people ask how I create and capture videos of ventilator waveforms. In this post I will describe my techniques and introduce a ventilator screen capture contest for my new book Ventilator Graphics: Identifying Patient Ventilator Asynchrony & Optimizing Settings (2nd Ed).
Here are the contest prizes:
- iTunes gift card ($50), free copy of the new book ($9.99), your screen shot will be used in the new book.
- iTunes gift card ($25) free copy of the new book ($9.99), your screen shot will be used in the new book.
- iTunes gift card ($10) free copy of the new book ($9.99), your screen shot will be used in the new book.
Labels:
Waveforms
Sunday, June 10, 2012
Why Aren't Your Patients Weaning? Don't Blame Nursing
 |
| http://respiratorytherapycave.blogspot.com/ |
The successful weaning and extubation of ventilated patients decreases hospital length of stay and reduces morbidity and mortality. One tool utilized to facilitate this process is “wean predictors” incorporated into RCP driven protocols to determine whether a patient may advance to a spontaneous breathing trial (SBT).
In a previous post [1] I mentioned that the level of sedation was the foremost reason why patients did not progress to a spontaneous breathing trial with a prevalence of 48%.
This is concerning since it is a standard of care to provide ventilator patients with a daily "sedation vacation" or a interruption or decrease in sedation to assess neurological status and wean readiness.
This poses many questions:
Labels:
Weaning
Friday, May 18, 2012
ECLS for Patient Ventilator Synchrony?
 |
| Extracorporeal Cardiopulmonary Life Support. Image from MAQUET |
Introduction
Increasing sedation and administering neuromuscular blocking agents increases the risk for ventilator induced diaphragmatic dysfunction (VIDD), increased length of stay, and mortality. So it would be ideal to allow for both lung protection and patient comfort (ventilator synchrony) with minimal sedation use.
In the below summarized abstract [1] researchers couple Extracorporeal Cardiopulmonary Life Support (ECLS) with Neurally Adjusted Ventilatory (NAVA) Assist to balance lung protection and patient comfort with little sedation use.
Saturday, May 12, 2012
The Importance of Identifying Patient Ventilator Asynchrony
One factor associated with PMV is inappropriate ventilator settings. The below abstract reinforces how ventilator asynchrony increases the likelihood of PMV.
Sunday, April 29, 2012
Electrolyte Imbalances During Mechanical Ventilation
Numerous factors contribute to ventilator dependence. However, one should focus on identifying factors that are potentially reversible. Electrolyte imbalances have a direct relationship to weaning from mechanical ventilation.
Below is a summary of different electrolytes and how their imbalances may prolong mechanical ventilation.
Labels:
Weaning
Sunday, April 15, 2012
Inhaled Nitric Oxide Set-up for Cardiac Surgery
Another use for inhaled nitric oxide is for lowering pulmonary vascular resistance during cardiothoracic surgery. Administration is common during mitral valve replacements, heart transplants, and implantation of left ventricular assist devices.
One concern is interfacing the INOVent with the anesthesia machine, primarily preventing "Nitric Dioxide" build up.
Here are the steps to interface the INOVent with the anesthesia machine:
One concern is interfacing the INOVent with the anesthesia machine, primarily preventing "Nitric Dioxide" build up.
Here are the steps to interface the INOVent with the anesthesia machine:
Sunday, April 8, 2012
The Worst Modes of Mechanical Ventilation
 |
| IMV one of the worst ventilator modes in regards to patient comfort. |
Many will argue the best mode of mechanical ventilation
and prefer the mode that is most commonly used in their patient populations.
Strict believers of the ARDS net protocol will favor VC-CMV to ensure lower
tidal volume delivery. Pediatric centers will insist on Pressure targeted modes
to limit high pressures, and trauma centers may favor biphasic modes of
ventilation to obtain higher mean airway pressures.
However, some institutions use the worst modes of
ventilation that directly impede on patient comfort. Promoting patient comfort
is one of the main goals of mechanical ventilation [1] and not providing
comfort may lead to over sedation, over ventilation, ventilator induced
diaphragmatic dysfunction, and increased length of stay.
So what are the worst modes of ventilation specifically
in regards to patient comfort?
Sunday, April 1, 2012
Inhaled Nitric Oxide Set-up for Nitric Oxide Challenge
One off label use of inhaled nitric oxide is to use it to see if a patients pulmonary hypertension is responsive to vasodilator therapy.
Due to inhaled nitric oxides quick onset and extremely short half life the "nitric oxide challenge" can be performed safely and efficiently in a cardiac cath lab.
There are a few standard protocols which I will not go over, however I will go over device and patient interface setup for performing a nitric oxide challenge.
Tuesday, March 27, 2012
Quantifying Patient Ventilator Asynchrony
 |
SERVO-i Ventilator screen. Using NAVA monitoring & captured screen shots to quantify patient ventilator asynchrony.
|
Patient ventilator asynchrony is present in the majority of ventilated patients [1].
One of the most difficult components of patient ventilator assessment is actually recognizing asynchrony. Authors of the following study “Efficacy of ventilator waveforms observation in detecting patient–ventilator asynchrony” ‘[2] demonstrate how challenging identifying asynchrony is, even for the seasoned physician.
Sunday, March 18, 2012
CPT Sham
Why do we keep on performing Chest Physical Therapy?
This recent Cochrane Database review reinforces that CPT does not improve outcomes [1].
Overview
This is a further update of the original Cochrane review published in 2005 and updated in 2007. Acute bronchiolitis is the leading cause of medical emergencies during winter in children younger than two years of age. The main objective of the study was to determine the efficacy of chest physiotherapy in infants aged less than 24 months old with acute bronchiolitis. A secondary objective was to determine the efficacy of different techniques of chest physiotherapy. The researchers searched various past studies including the Cochrane Central Register of Controlled Trials (CENTRAL) which contains the Cochrane Acute Respiratory Infections Group's Specialized Register. Selection included randomized controlled trials (RCTs) in which chest physiotherapy were compared against no intervention or against another type of physiotherapy in bronchiolitis patients younger than 24 months of age. Finally, two review authors independently extracted data. The primary outcomes included respiratory parameters and improvement in severity of disease. The secondary outcomes included length of hospital stay, duration of oxygen supplementation and the use of bronchodilators and steroids. No pooling of data was possible.
Labels:
CPT
Thursday, March 1, 2012
The Minimal SSI Strategy
 | ||
| Stress Index (Si) Displayed on the SERVO-i Ventilator. |
In 2009 Brunner & Wysocki proposed that there is an optimal breathing pattern to minimize stress & strain during mechanical ventilation [1]. Stress and strain are primary causes of ventilator induced lung injury (VILI), so it would be imperative to provide a breathing pattern which decreases the chances of VILI.
Monday, February 27, 2012
Wednesday, February 22, 2012
Monday, February 6, 2012
"It's a Nail"
 |
“Spoils of War” by Andy Ihnatko 2009.
A colleague of mine described a presentation she attended today in which the speaker was describing the usefulness of the “Dynamic Lung” and how there was no use for those squiggly little lines (referring to ventilators waveforms).
Is this guy serious? |
Labels:
Waveforms
Monday, January 9, 2012
Wednesday, November 30, 2011
Tuesday, November 22, 2011
APRV in the Operating Room is it Practical?
Airway Pressure Release Ventilation in the Operating Room is it Practical?
This is a good question, for one anesthesia delivery systems do not have APRV as a mode of ventilation available, so an ICU ventilator will need to be transported with the patient to the operating room.
Other considerations include:
-General anesthesia
-Hypo-ventilation
-Hypoxia
For more view the attached video
This is a good question, for one anesthesia delivery systems do not have APRV as a mode of ventilation available, so an ICU ventilator will need to be transported with the patient to the operating room.
Other considerations include:
-General anesthesia
-Hypo-ventilation
-Hypoxia
For more view the attached video
Labels:
APRV
Thursday, November 10, 2011
A Unique Way to Obtain the NIF
There are multiple ways to obtain the Negative Inspiratory Force (NIF) NIP (negative inspiratory pressure), or MIP (maximal inspiratory pressure) measurement. The NIF “corresponds to the negative pressure generated by the inspiratory muscles during a maximal inspiratory effort, performed during temporary occlusion of the airway opening” [1]. This parameter is used to quantify that the respiratory drive is sufficient (paralytics, narcotics, sedation is worn off after general anesthesia) or that there is no respiratory muscle fatigue or exhaustion.
 |
| Using the trigger setting to quantify extubation readiness. Notice the measured PEEP value & set PEEP value, the patient is able to generate a NIF < -18 cmH2O. |
There are multiple ways to obtain the Negative Inspiratory Force (NIF) NIP (negative inspiratory pressure), or MIP (maximal inspiratory pressure) measurement. The NIF “corresponds to the negative pressure generated by the inspiratory muscles during a maximal inspiratory effort, performed during temporary occlusion of the airway opening” [1]. This parameter is used to quantify that the respiratory drive is sufficient (paralytics, narcotics, sedation is worn off after general anesthesia) or that there is no respiratory muscle fatigue or exhaustion.
Thursday, September 29, 2011
Waveform of the Week: “Golden Moment”
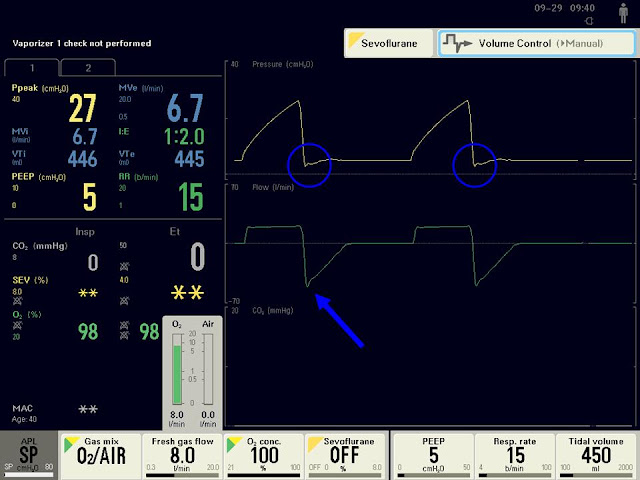 | |||||||||||||||
| Image 1: Screen of the FLOWi anesthesia delivery system, showing the "Golden Moment" highlighted with blue circle. |
It has been over a year since writing a waveform of the week post; however I have incorporated ventilator waveform pictures in recent posts. The waveform for this week is termed the “Golden Moment”
Labels:
Waveforms
Monday, September 19, 2011
Decreasing Dyspnea during Mechanical Ventilation
 | |||||||
| Flow Mismatch Associated with VC-CMV |
Utilizing Volume Control-Continuous Mandatory Ventilation (VC-CMV) may lead to patient ventilator asynchrony [1] and dyspnea. The main reason for these issues is the fixed (constant) flow rate associated with VC-CMV.
Labels:
Waveforms
Sunday, September 4, 2011
Automatic Setting of T-Low during Airway Pressure Release Ventilation: Is it Beneficial?
 |
| http://www.draeger.com/UK/en/products/medical_ventilation/adult_icu_ventilation/rsp_evita_infinity_v500_sw2.jsp |
Setting T-Low during APRV (a.k.a. Bi-Level, Bi-Vent) can be confusing and time consuming, to make it even more complicated there are three published techniques on how to set T-Low [1].
One method is setting T-Low based on the measured peak expiratory flow rate [2, 3]. The new Draeger Evita Infinity V500 ventilator allows the operator to set an “Auto-release” based on zero (0)-to- 80% of the Peak expiratory flow. This feature is nice since the operator does not have to continually assess the waveform &titrate the T-Low setting.
Conversely, this may be the least effective way to set T-Low in regards to lung protective goals, due to the inconsistent exhaled tidal volumes & auto-PEEP created with this technique [4].
Reference
[1]. Siddiqul,M. et.al.(2010). Comparison of Three Methods to Set T-Low on Airway Pressure Release Ventilation: A Model Study. Respiratory Care. 2010
[2]. Richey, S. (2009). Optimal T-Low Settings.
[3]. Richey, S. (2010). A Quick & Easy Way to Set T-Low During Airway Pressure Ventilation. http://kscottrichey.blogspot.com/2010/12/quick-precise-way-to-set-t-low-during.html
[4]. Richey, S. (2011). Setting T-Low During Airway Pressure Release Ventilation to Achieve Lung Protective Goals. http://kscottrichey.blogspot.com/2011/08/setting-t-low-during-airway-pressure.html
Labels:
APRV
Subscribe to:
Posts (Atom)



