In a previous post "APRV in the operating room is it
practical?" I argue that bringing a
ICU ventilator into the operating room to utilize APRV is not practical and may
lead to hypoventilation and hypoxia due to administration of anesthetic agents
[1].
During surgical procedures the patient is maintained in
stage 3 of anesthesia known as the "surgical stage". Stage 3 is
broken down into four distinct planes, "from onset of automatic
respiration to respiratory paralysis" [2]. The patient is usually maintained
in Plane 3 (intercostal muscle paralysis) or Plane 4 (diaphragmatic paralysis)
leading to the cessation of spontaneous breaths.
One key advantage of APRV is that the patient may breathe
spontaneously contributing to the overall minute volume, with the termination of
spontaneous efforts the patient will become severely hypercapnic.
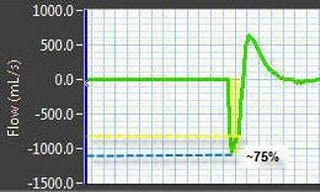
Below is an image (fig 1) I captured from a "Pressure
Control Ventilation Simulator" [3] demonstrating an ARDS patient on APRV.
 |
| Figure 1. Pressure Control Ventilation Simulator, notice patients PaCO2 at 100.7 mmHg. |
Another example of how APRV maybe harmful in the operating room is when trying to mimic APRV with a anesthesia delivery system.