Free Bronchoscopy Simulator
Wednesday, November 30, 2011
Tuesday, November 22, 2011
APRV in the Operating Room is it Practical?
Airway Pressure Release Ventilation in the Operating Room is it Practical?
This is a good question, for one anesthesia delivery systems do not have APRV as a mode of ventilation available, so an ICU ventilator will need to be transported with the patient to the operating room.
Other considerations include:
-General anesthesia
-Hypo-ventilation
-Hypoxia
For more view the attached video
This is a good question, for one anesthesia delivery systems do not have APRV as a mode of ventilation available, so an ICU ventilator will need to be transported with the patient to the operating room.
Other considerations include:
-General anesthesia
-Hypo-ventilation
-Hypoxia
For more view the attached video
Labels:
APRV
Thursday, November 10, 2011
A Unique Way to Obtain the NIF
There are multiple ways to obtain the Negative Inspiratory Force (NIF) NIP (negative inspiratory pressure), or MIP (maximal inspiratory pressure) measurement. The NIF “corresponds to the negative pressure generated by the inspiratory muscles during a maximal inspiratory effort, performed during temporary occlusion of the airway opening” [1]. This parameter is used to quantify that the respiratory drive is sufficient (paralytics, narcotics, sedation is worn off after general anesthesia) or that there is no respiratory muscle fatigue or exhaustion.
 |
| Using the trigger setting to quantify extubation readiness. Notice the measured PEEP value & set PEEP value, the patient is able to generate a NIF < -18 cmH2O. |
There are multiple ways to obtain the Negative Inspiratory Force (NIF) NIP (negative inspiratory pressure), or MIP (maximal inspiratory pressure) measurement. The NIF “corresponds to the negative pressure generated by the inspiratory muscles during a maximal inspiratory effort, performed during temporary occlusion of the airway opening” [1]. This parameter is used to quantify that the respiratory drive is sufficient (paralytics, narcotics, sedation is worn off after general anesthesia) or that there is no respiratory muscle fatigue or exhaustion.
Thursday, September 29, 2011
Waveform of the Week: “Golden Moment”
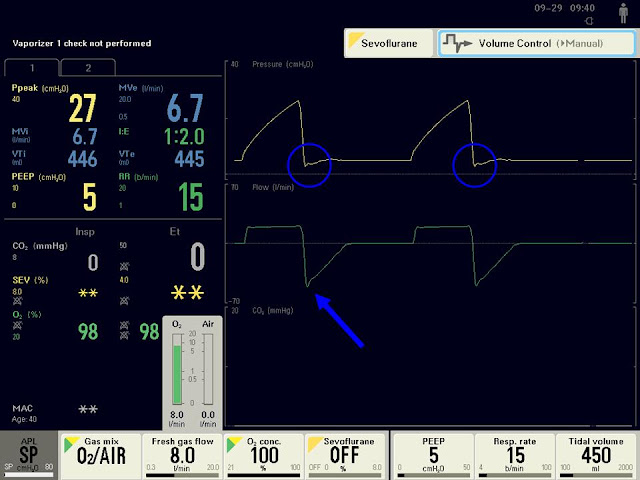 | |||||||||||||||
| Image 1: Screen of the FLOWi anesthesia delivery system, showing the "Golden Moment" highlighted with blue circle. |
It has been over a year since writing a waveform of the week post; however I have incorporated ventilator waveform pictures in recent posts. The waveform for this week is termed the “Golden Moment”
Labels:
Waveforms
Monday, September 19, 2011
Decreasing Dyspnea during Mechanical Ventilation
 | |||||||
| Flow Mismatch Associated with VC-CMV |
Utilizing Volume Control-Continuous Mandatory Ventilation (VC-CMV) may lead to patient ventilator asynchrony [1] and dyspnea. The main reason for these issues is the fixed (constant) flow rate associated with VC-CMV.
Labels:
Waveforms
Sunday, September 4, 2011
Automatic Setting of T-Low during Airway Pressure Release Ventilation: Is it Beneficial?
 |
| http://www.draeger.com/UK/en/products/medical_ventilation/adult_icu_ventilation/rsp_evita_infinity_v500_sw2.jsp |
Setting T-Low during APRV (a.k.a. Bi-Level, Bi-Vent) can be confusing and time consuming, to make it even more complicated there are three published techniques on how to set T-Low [1].
One method is setting T-Low based on the measured peak expiratory flow rate [2, 3]. The new Draeger Evita Infinity V500 ventilator allows the operator to set an “Auto-release” based on zero (0)-to- 80% of the Peak expiratory flow. This feature is nice since the operator does not have to continually assess the waveform &titrate the T-Low setting.
Conversely, this may be the least effective way to set T-Low in regards to lung protective goals, due to the inconsistent exhaled tidal volumes & auto-PEEP created with this technique [4].
Reference
[1]. Siddiqul,M. et.al.(2010). Comparison of Three Methods to Set T-Low on Airway Pressure Release Ventilation: A Model Study. Respiratory Care. 2010
[2]. Richey, S. (2009). Optimal T-Low Settings.
[3]. Richey, S. (2010). A Quick & Easy Way to Set T-Low During Airway Pressure Ventilation. http://kscottrichey.blogspot.com/2010/12/quick-precise-way-to-set-t-low-during.html
[4]. Richey, S. (2011). Setting T-Low During Airway Pressure Release Ventilation to Achieve Lung Protective Goals. http://kscottrichey.blogspot.com/2011/08/setting-t-low-during-airway-pressure.html
Labels:
APRV
Friday, August 26, 2011
Change Your Ventilator Management
In last months article “Effects of Implementing Adaptive Support Ventilation in a Medical Intensive Care Unit” in the Respiratory Care Journal [1], Chew & colleagues discovered that ASV provided a quicker time to extubation readiness then their standard ventilation protocol.
These results are not surprising, especially after reviewing their standard way of managing ventilator patients. This study was a poor comparison of practitioner guided ventilator management versus an automated ventilator mode.
Let’s compare & contrast the differences in the ASV study group versus the traditional ventilator management there are three (3) main areas to investigate.
Thursday, August 11, 2011
Setting T-Low during Airway Pressure Release Ventilation to Achieve Lung Protection Goals
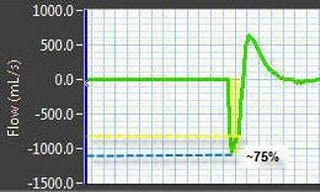 |
| Setting a T-Low based on a 50-75% PEFR may contribute to excessive exhaled tidal volumes |
There are three published techniques to set T-Low when utilizing Airway Pressure Release Ventilation (APRV) or mimicking (BiVent, BiLevel) the application.
They include:
Labels:
APRV
Sunday, July 24, 2011
Adaptive Support Ventilation: Set it & forget it?
 |
| http://blog.poplabs.com/2008/07/set-it-and-forget-it-why-roncos-showtime-rotisserie-cant-run-your-marketing-campaign/
I once mentioned in a previous posting (Adaptive Support Ventilation: the Pareto Principle of Mechanical Ventilation) that “
This is not a Ronco Rotisserie Oven ® this is a mechanical ventilator and the operator needs to be engaged and assess patient-ventilator interaction.
Here are some areas of focus:
|
Sunday, July 17, 2011
Switching from Pressure Control to Volume Control Ventilation
During patient ventilator transports one may have to switch from pressure control (PC-CMV) to volume control (VC-CMV) ventilation, because the available transport ventilator does not have PC-CMV. Another reason is the operator is unfamiliar with PC-CMV.
Here are the steps and additional considerations to safely switch the patient over.
Sunday, July 10, 2011
Obtaining Pulmonary mechanics with the PB840 Ventilator
In my opinion I believe the PB840 ventilator is an outdated platform. One thing that frustrates me is that additional functions/features cost the purchaser extra, where on most ventilators these functions are standard.
Examples:
-Trending
-P0.1
-No low flow lung mechanics tool.
The only thing I believe is useful is Proportional Assist Plus, however this is still a software upgrade charge.
Another frustration when using the PB840 is obtaining pulmonary mechanics measurements correctly.
When properly obtaining these measurements one has to place the patient in VC-CMV (volume controlled ventilation) and perform an additional three steps.
Here are the steps:
1. Place the patient in VC mode (if the patient is in another mode)
2. Change the flow waveform setting to a Square (constant) flow waveform pattern.
3. Change the flow setting value to obtain a I-time which matches the previous set I-time.
4. Perform an inspiratory pause, by pressing the inspiratory pause button (insp pause)
Sunday, July 3, 2011
Capnography the Importance of Perfusion
Capnography/ETCO2 monitoring (ETCO2) has been used for many years in the operating room to confirm endo-tracheal tube placement and to evaluate the patient’s ventilatory status. Since the technology has become more portable and affordable, it has migrated to intensive care units, emergency rooms, ambulances, and even step down units. Due to this prevalence Capnography/End-tidal carbon dioxide monitoring is becoming the “fifth” vital sign [1].
Wednesday, June 29, 2011
Sun Glasses at Night?
 |
| http://en.wikipedia.org/wiki/Sunglasses_at_Night In his 1984 single “Sunglasses at Night” singer Corey Hart sings about wearing his sun glasses to watch his lover, as she lies and cheats on him or this is what I think the lyrics mean? I’m not one to decipher song lyrics; I just thought it was a pretty catchy tune when it was first released. Wearing sun glasses at night seems pretty idiotic, but what about night shift workers wearing sun glasses? |
Labels:
commentary
Saturday, June 25, 2011
4 Reasons Not to Use APRV
 |
| Over Inflated |
Airway Pressure Release Ventilation is a modality of ventilation that has been in use for greater than 20 years. Some practitioners' believe APRV is the panacea of mechanical ventilation and utilize the mode on every ventilated patient. Before initiating APRV one should consider 4 arguments against its use.
Labels:
APRV
Wednesday, June 22, 2011
Performing a T-Piece Trial with the Ventilator
 |
| Utilizing the Pressure/Volume Loop to determine the appropriate pressure support level during a simulated T-piece trial. |
Many institutions perform spontaneous breathing trials with the ventilator using a small amount of PEEP (~ 5 cmH2O) and automatic tube compensation or a small amount of pressure support (~ 5 to 10 cmH2O). However, occasionally a traditional T-Piece trial may prove to be more beneficial [1].
Utilizing pressure support during a spontaneous breathing trial to off-set the work of breathing related to the artificial airway may lead to false positives, due to over compensation.
Why is this?
Labels:
Weaning
Friday, June 10, 2011
Saturday, June 4, 2011
SmartCare PS: Concerns with Delayed Cycling
SmartCare/PS® or SmartCare Pressure support (™ Draeger Medical, Telford , PA United States
Smartcare is a spontaneous mode of ventilation (CSV), which uses pressure support to augment the inspiratory efforts. The operator is allowed to change the pressurization rate (rise time), however has no control of the “Expiratory Cycling Threshold” which is one of the determinates of how a pressure support breath ends.
A Review of Pressure Support Termination
Labels:
SmartCare
Saturday, May 28, 2011
The Utilization of Mid-Frequency Ventilation with a Sophisticated Transport Ventilator: a Case Study
Background
Mid-Frequency Ventilation was first described in the medical literature by Mireles-Cabodevila & Chatburn in 2008 [1]. The authors describe Mid-Frequency Ventilation (MFV) as setting ventilator frequencies greater than 35 cycles per minute, during Pressure Control-Continuous Mandatory Ventilation (PC-CMV) to provide increased minute ventilation support in patients with severe Acute Respiratory Distress Syndrome (ARDS). In this initial article the authors tested their theory on both a computer simulation model and bench study using newer generation conventional intensive care unit ventilators. Both test simulations where successful.
In 2010 Mireles-Cabodevila & al. applied the theory in a live neonatal & pediatric animal model; the results reinforced the previous hypothesis showing the potential benefits of MFV [2].
As of to date there have been no cases reported in the medical literature of MFV being applied in humans. I previously presented a case where MFV was applied for a patient with serve hypercapnia; however this was never submitted for publication [3].
The following case involves using MFV on a sophisticated transport ventilator, thus reinforcing the versatility of MFV. The operator does not need a special ventilator (e.g. oscillator) or mode (e.g. APRV). Even though one does not need a specific ventilator the device still needs to safely and effectively ventilate injured lungs. The transport ventilator used during this case is considered a “sophisticated” transport ventilator, one that can effectively ventilate injured lungs [4].
Mid-Frequency Ventilation was first described in the medical literature by Mireles-Cabodevila & Chatburn in 2008 [1]. The authors describe Mid-Frequency Ventilation (MFV) as setting ventilator frequencies greater than 35 cycles per minute, during Pressure Control-Continuous Mandatory Ventilation (PC-CMV) to provide increased minute ventilation support in patients with severe Acute Respiratory Distress Syndrome (ARDS). In this initial article the authors tested their theory on both a computer simulation model and bench study using newer generation conventional intensive care unit ventilators. Both test simulations where successful.
In 2010 Mireles-Cabodevila & al. applied the theory in a live neonatal & pediatric animal model; the results reinforced the previous hypothesis showing the potential benefits of MFV [2].
As of to date there have been no cases reported in the medical literature of MFV being applied in humans. I previously presented a case where MFV was applied for a patient with serve hypercapnia; however this was never submitted for publication [3].
The following case involves using MFV on a sophisticated transport ventilator, thus reinforcing the versatility of MFV. The operator does not need a special ventilator (e.g. oscillator) or mode (e.g. APRV). Even though one does not need a specific ventilator the device still needs to safely and effectively ventilate injured lungs. The transport ventilator used during this case is considered a “sophisticated” transport ventilator, one that can effectively ventilate injured lungs [4].
Wednesday, May 25, 2011
Chest Physical Therapy Catastrophes
 |
| http://respiratorytherapycave.blogspot.com/ |
Background
Chest Physical Therapy (CPT) is ordered at many institutions for numerous conditions, from patients with chronic respiratory conditions-to-Acute Respiratory Distress Syndrome. The main goal of these therapies is to augment secretion mobilization & airway clearance[1]. Even though CPT is ordered liberally it does have associated risks and there is no supporting evidence that CPT is more valuable than a direct cough (Schans, 2007). At one institution I work at there have been 4 adverse events related to CPT in a short six month time span. I previously described two of the incidences on the same patient in the posting “Shook to Death: a Case Study of High-Frequency Chest Wall Compression”. The other two cases will be presented.
Case 1
An 83 year old patient whose initial compliant was for abdominal pain and nausea and vomiting. The patient was ordered CPT via Vest every four hours for unknown reasons (probably because the physician observed COPD in then dictated medical history). The patient’s pre-existing medical history included COPD, atrial fibulation, and left lung resection. CPT was initiated and the patient immediately went into atrial fib, the therapy was stopped to make sure the vibrations did not cause an inappropriate reading of the ECG. The A-fib remained present after stopping the CPT and the patient had to be medically treated for her symptoms. Thus increasing her ICU observation period.
Case 2
A 60 year old female patient admitted for respiratory distress was ordered CPT via percussion secondary to a left lower lobe infiltrate. The patients pre-existing medical history included cardiomyopathy, diabetes, hypertension, chronic renal insufficiency.
During the CPT procedure the patient experienced cardiopulmonary arrest, secondary to mucus plugging. The patient was resuscitated, placed on mechanical ventilation, and bronchoscopy was performed the following day. The patient had a lengthy intensive care unit stay and was eventually discharged.
Summary
CPT is a commonly prescribed therapy, with little evidence of success. Practitioners’ should be aware of the risk factors associated CPT and screen patients appropriately for their ability to clear the mobilized secretions. Always, consider if there is a rational for CPT and which therapy is likely to provide the greatest benefit with the least amount of harm.
[1] Schans, C. (2007). Conventional Chest Physical Therapy for Obstructive Lung Disease. Respiratory Care. 52 (9): 1198.
Labels:
CPT
Sunday, May 22, 2011
Ten Reasons to Trade in the Babylog 8000
 |
| Image 1 : Front view of the Babylog 8000 neonatal ventilator. |
The Babylog 8000™ (Draeger Medical, Telford , PA
The rationale for replacing the Babylog is related to technological advances, the lack of upgrade availability, and safety concerns.
Wednesday, May 18, 2011
Airway Obstruction Secondary to Growing Granulomatous Tissue in the Tracheostomy Tube
Introduction: Airway patency is arguably the most important factor of the cardiopulmonary system. It is imperative that the bedside Respiratory Care Practitioner (RCP) can rapidly detect and treat airway emergencies. One tool for assisting the RCP in detecting airway displacements and obstructions is the use of capnography. At our institution capnography is routinely used for confirmation of tracheostomy placement following tube placement or tube changes. This case study presents the effectiveness of capnography for detecting a partial airway obstruction with the correct placement of the tracheostomy tube.
Sunday, May 15, 2011
The Intrinsic Diaphragmatic Frequency
 |
Image 1: Missed trigger attempts, notice the flow distortions (purple flow waveform) without associated breaths. Ventilator measured rate 12 bpm, however true intrinsic rate 30 bpm.
|
Many patients receiving mechanical have high intrinsic diaphragmatic rates (≥30 breaths per minute) even when very well assisted [1]. This is usually unnoticed because the ventilator only measures machine or patient triggered breaths; however the patient’s true respiratory rate may be higher. This can be problematic when performing a spontaneous breathing trial (SBT) for a couple of reasons.
Labels:
Waveforms
Wednesday, May 11, 2011
Adaptive Pressure Control Ventilation and Severe Sepsis a Grueling Combination
Mentioned in previous postings Adaptive Pressure Control (APC ) should be used cautiously in patients with high inspiratory drives. In patients with sepsis APC can become problematic by weaning the driving pressure prematurely due to a vigorous respiratory drive associated with lactic acidosis. The lower driving pressures will not efficiently off load the respiratory muscles leading to increased work of breathing, ventilatory muscle fatigue, and may initiate lung injury.
Provided are two examples of APC utilized in sepsis patients:
Sunday, May 8, 2011
The Least Work of Breathing: Applying principles of Adaptive Support Ventilation
Adaptive Support Ventilation (ASV) is an advanced closed-loop mode of ventilation only available on Hamilton Medical ventilators (G5, Galileo, C2) in the United States.
ASV is considered an “Optimal” mode of ventilation, in which the ventilator automatically adjusts multiple set-points (pressure, tidal volume, frequency, & I: E ratio). Furthermore, the ventilator applies a mathematical model (Otis equation) to find the least work of breathing.
Providing minimal work of breathing is a primary goal for the mechanically ventilated patient. A load that is too high will eventually lead to ventilatory muscle fatigue and may lead to lung injury and/or liberation failure. Every practitioner should attempt to minimize the work of breathing (WOB) by continuously assessing the patient ventilator interaction and adjusting settings appropriately.
If available the practitioner could employ ASV, however what if you don’t have a Hamilton ventilator or unfamiliar with ASV?
ASV is considered an “Optimal” mode of ventilation, in which the ventilator automatically adjusts multiple set-points (pressure, tidal volume, frequency, & I: E ratio). Furthermore, the ventilator applies a mathematical model (Otis equation) to find the least work of breathing.
Providing minimal work of breathing is a primary goal for the mechanically ventilated patient. A load that is too high will eventually lead to ventilatory muscle fatigue and may lead to lung injury and/or liberation failure. Every practitioner should attempt to minimize the work of breathing (WOB) by continuously assessing the patient ventilator interaction and adjusting settings appropriately.
If available the practitioner could employ ASV, however what if you don’t have a Hamilton ventilator or unfamiliar with ASV?
Wednesday, May 4, 2011
The RT Hoarder
 |
| http://cache.gawker.com/assets/images/gawker/2009/10/cats.jpg |
I admit I have turned into a hoarder, not the typical hoarder seen on television living amongst their bodily waste or sharing their house with 50 cats. My story is not as disturbing and goes unnoticed.
Labels:
Business
Wednesday, April 27, 2011
Dead of Night shift
 | |||
| http://en.wikipedia.org/wiki/File:DeadOfNight1.jpg |
After six years of being a day walker I have returned to my origin as a night shift healthcare provider. I enjoy the pace and the autonomy of night shift however, it is sometimes torturous.
I feel like “Walter Craig” in the 1945 British film “Dead of Night”, in which the character experiences a recurring nightmare with the same cast of house guests. Instead of “Pilgrims Farm” I’m stuck in a hospital interacting with it's own recurring cast of personalities; the non-compliant patient, the substance abuse patient, the medical resident who thinks he’s M.D. “House”, the nurses who are fueled on cigarettes & Red Bull. Yes, I’m dead of night shift; indifferent, cold, and apathetic. Additionally, night shift is slowly killing me.
Night shift work has been associated with a number of maladies including:
Metabolic syndrome [1& 2]
Increased vascular stress [3 & 4]
Induced Apnea [5]
In regards to me it is vitamin D deficiency. Yearly, I have a few blood tests performed to check for abnormal values. Before returning to night shift my previous vitamin D levels were normal, I lived in the Midwest, and had no additional vitamin D supplementation. After starting night shift I began supplementing my vitamin D intake with 1000 micro units/day & I also moved to the east coast (more sun), conversely my results were below normal. I always have these test performed in February, so the amount of sunlight/day/month is not a factor.
[1] Biggi, N. et. Al. (2008). Metabolic Syndrome in Permanent Night Shift Workers. Chronobiol Int.
[2] Pietroiusti, A. et. Al. (2010). Incidence of Metabolic Syndrome Among Night-Shift Healthcare Workers. Occup Environ Med.
[3] Lo, SH. et.al. (2010). Working Night Shift Causes Increased Vascular Stress and Delayed Recovery in Young Women. Chronobiol Int.
[4] McCubbin, JA. et. Al. (2010). Blood Pressure Increases During a Simulated Night Shift in Persons at Risk for Hypertension. Int J Behav Med.
[5] Laudencka, A. et. Al. (2007). Does Night-Shift Work Induce Apnea Events in Obstructive Sleep Apnea Patients? J Physiol Pharmacol.
Labels:
commentary
Sunday, April 24, 2011
Setting Ventilator Alarms Diagnostically
Many practitioners set alarm thresholds thoughtlessly due to the fact that many ventilators do a poor job of filtering alarm nuisances versus 'high-risk' alarms. Many times I see the high respiratory rate alarm set at threshold in which the patient would have severe air trapping and dynamic hyperinflation before the alarm threshold is met.
When using controlled modes of ventilation (VC-CMV & PC-CMV) it is extremely important to set the high respiratory rate alarm threshold appropriately.
During both machine and patient initiated breaths the inspiratory time is fixed, so any additional breaths takes away from the expiratory time which can quickly lead to a inverse inspiratory-to-expiratory (I: E) ratios.
How to set the High Respiratory Rate Alarm Diagnostically
In patients with obstructive airway disease I prefer to set my high
respiratory rate based on a 1:1, I: E ratio.
That is when the patient sets off the high respiratory rate alarm I know that they are breathing at a 1:1 ratio and that any additional breaths will be an inverse I: E ratio, putting the patient at a increased risk for dynamic hyperinflation.
This is easy to calculate based on the patient's set inspiratory time.
Formula: x = 60/(I-time * 2)
X (high respiratory rate alarm)
60 (total cycle time)
I-time (machine set I-time)
A common I-time is 1.0 second this would equal a high respiratory rate alarm of 30 breaths/minute. This stays the same if the set rate is 8 or 25; the 1:1 threshold is at 30 breaths/min.
The 0.25 Second difference
If air trapping is a concern just decrease the I-time.
A 0.25 second change is significant.
Decreasing the I-time from 1.0 second to 0.75 second increases the
alarm threshold to 40 bpm.
When using controlled modes of ventilation (VC-CMV & PC-CMV) it is extremely important to set the high respiratory rate alarm threshold appropriately.
During both machine and patient initiated breaths the inspiratory time is fixed, so any additional breaths takes away from the expiratory time which can quickly lead to a inverse inspiratory-to-expiratory (I: E) ratios.
How to set the High Respiratory Rate Alarm Diagnostically
In patients with obstructive airway disease I prefer to set my high
respiratory rate based on a 1:1, I: E ratio.
That is when the patient sets off the high respiratory rate alarm I know that they are breathing at a 1:1 ratio and that any additional breaths will be an inverse I: E ratio, putting the patient at a increased risk for dynamic hyperinflation.
This is easy to calculate based on the patient's set inspiratory time.
Formula: x = 60/(I-time * 2)
X (high respiratory rate alarm)
60 (total cycle time)
I-time (machine set I-time)
A common I-time is 1.0 second this would equal a high respiratory rate alarm of 30 breaths/minute. This stays the same if the set rate is 8 or 25; the 1:1 threshold is at 30 breaths/min.
The 0.25 Second difference
If air trapping is a concern just decrease the I-time.
A 0.25 second change is significant.
Decreasing the I-time from 1.0 second to 0.75 second increases the
alarm threshold to 40 bpm.
Labels:
Other
Wednesday, April 20, 2011
Low Peak Inspiratory Pressures During Adaptive Pressure Control Ventilation: an Indication for Weaning
Low Peak Inspiratory Pressures (PIP) during Adaptive Pressure Control (APC) may be a sign of distress in patients with increased inspiratory efforts (e.g. high metabolic rate, sepsis, and hypercapnea) [1], or may be a sign that the patient is ready for spontaneous breathing trials.
In the patient that is not in distress and the PIP is low (≤ 15 cmH20) consider evaluation for liberation. If the PIP is low one can presume that the patients’ pulmonary mechanics have improved or within the normal range and that the workload imposed by low compliances or high resistances have decreased.
Example Case
80 female patient with the following ventilator settings:
Mode- APC, Rate- 12, Vt- 500, Fio2- 35%, PEEP- +5 cmH2O
Discovered from the ventilator patient assessment that the patient’s PIP was only 13 cmH2O and the patient was resting comfortably. At this institution spontaneous breathing trials are performed with CSV-PS, Pressure Support of 7 cmH2O & a PEEP +5 (PIP total 12 cmH2O).
The measured PIP over the previous 48 hours was a ~ mean of 13 cmH2O.
This was significant, the patient was basically on the same control pressure as what this facility does SBT’s on, indicating that the patient should have been weaned or liberated 48 hours earlier.
After this finding the patient was immediately placed on a Trach collar trial. The trial was successful with no complications and the patient was transferred to a general medical floor within 48 hours.
Conclusion
Low PIP during APC ventilation should always be evaluated further for the potential for liberation from mechanical ventilation or the need for adjusting ventilator settings to decrease the work of breathing.
[1] The Problem With Adaptive Pressure Control Modes of Ventilation: a Case Study.
In the patient that is not in distress and the PIP is low (≤ 15 cmH20) consider evaluation for liberation. If the PIP is low one can presume that the patients’ pulmonary mechanics have improved or within the normal range and that the workload imposed by low compliances or high resistances have decreased.
Example Case
80 female patient with the following ventilator settings:
Mode- APC, Rate- 12, Vt- 500, Fio2- 35%, PEEP- +5 cmH2O
Discovered from the ventilator patient assessment that the patient’s PIP was only 13 cmH2O and the patient was resting comfortably. At this institution spontaneous breathing trials are performed with CSV-PS, Pressure Support of 7 cmH2O & a PEEP +5 (PIP total 12 cmH2O).
The measured PIP over the previous 48 hours was a ~ mean of 13 cmH2O.
This was significant, the patient was basically on the same control pressure as what this facility does SBT’s on, indicating that the patient should have been weaned or liberated 48 hours earlier.
After this finding the patient was immediately placed on a Trach collar trial. The trial was successful with no complications and the patient was transferred to a general medical floor within 48 hours.
Conclusion
Low PIP during APC ventilation should always be evaluated further for the potential for liberation from mechanical ventilation or the need for adjusting ventilator settings to decrease the work of breathing.
[1] The Problem With Adaptive Pressure Control Modes of Ventilation: a Case Study.
Sunday, April 17, 2011
Delayed Cycling
One form of delayed cycling is when the operator inappropriately sets the inspiratory time too
long.
long.
However, delayed cycling is also very common during CSV-PS.
A pressure spike at the end of inspiration may indicate delayed cycling however this is not always associated with expiratory muscle activity . The spike may also be due to the relaxation of the inspiratory muscles, the spike is caused by the returning of pressure creating a temporary increase in pressure (usually associated with higher levels of pressure support > 10 cmH2O).
A pressure spike at the end of inspiration may indicate delayed cycling however this is not always associated with expiratory muscle activity . The spike may also be due to the relaxation of the inspiratory muscles, the spike is caused by the returning of pressure creating a temporary increase in pressure (usually associated with higher levels of pressure support > 10 cmH2O).
Always evaluate the patient for distress to determine if it is delayed cycling vs. muscle relaxation. If the patient looks relaxed and the P0.1 is within limits then the spike is most likely due to muscle relaxation.
A 25% expiratory cycling threshold is a common default setting in most mechanical ventilators. This setting is appropriate in a large percent of the patient population. As previously mentioned a default setting of 25% may be too short in patients recovering from ALI, conversely , in patients with histories of airway obstruction this setting may be too long.
Prolonged expiratory cycling in the COPD patient may increase work of breathing, intrinsic PEEP, and trigger asynchronies (ineffective efforts).Waveform book at
Prolonged expiratory cycling in the COPD patient may increase work of breathing, intrinsic PEEP, and trigger asynchronies (ineffective efforts).Waveform book at
Labels:
Waveforms
Saturday, April 16, 2011
Is the T-Piece Trial Futile? 3 Cases that Justify a T-Piece Trial.
In a current Blog posting “No More T-Piece” author Rick Frea states that at his facility T-piece trials are pretty much non-existent.
I don’t remember the last time I have preformed a T-piece trial on a patient with an E.T. Tube? It is very popular these days to perform the Spontaneous Breathing Trial (SBT) inline with the mechanical ventilator, due to the advance physiological monitoring and the extra alarm capabilities.
Most institutions I’m familiar with use a small amount of pressure support (~5 cmH2O) or Automatic Tube Compensation (a.k.a. Tube Comp, ATC, or Tube Resistance Compensation) if it is available on the machine to overcome the resistance of the artificial airway.
Even though the t-piece method is rarely used I believe it can be beneficial and more diagnostic in some cases to prevent false positives created by spontaneous breathing augmented with pressure support & PEEP.
3 examples:
Labels:
Weaning
Sunday, April 10, 2011
Premature Cycling
 | ||||
| Image 1: Patient coughing, notice the peak pressure spikes (yellow pressure waveform) this may lead to premature cycling. |
Premature Cycling
Premature cycling also known as premature termination or short cycling occurs when the ventilator breath cycle ceases abruptly, while the patient requires a longer inspiratory phase. It is defined by the delivered inspiratory time is less than 50% of the mean inspiratory time [1,2].
Premature cycling also known as premature termination or short cycling occurs when the ventilator breath cycle ceases abruptly, while the patient requires a longer inspiratory phase. It is defined by the delivered inspiratory time is less than 50% of the mean inspiratory time [1,2].
Premature cycling may be attributed to pressure over-shots, causing the breath to cycle-off when the generated pressure meets the safety threshold setting. A good example of this is when a patient coughs during volume controlled ventilation (VC-CMV, VC-SIMV), in which the exhalation valve is closed throughout the set inspiratory time.
Labels:
Waveforms
Sunday, April 3, 2011
Adaptive Support Ventilation: the “Pareto Principle” of Mechanical Ventilation.
One reader asked me “what do you think about ASV” (Adaptive Support Ventilation) in which I replied back “I think it is the Pareto Principle or Pareto Efficiency of mechanical ventilation”.
So what is the Pareto Principle?
So what is the Pareto Principle?
Friday, April 1, 2011
Oral Exam: 99.9 % Failure Rate Among ICU Nurses
Question 1. What is pictured in image 1?
 | |||
| Image 1 |
Question 2. What is it used for?
If you answered “Bite Block” you must be an ICU nurse.
I cannot count how many times nurses have tried to use the “oropharyngeal airway” as a bite block and complain about how the patient is fighting the tube & airway, gagging, and fighting the ventilator.
The next step, they usually heavily sedate or paralyze the patient.
An oropharyngeal airway is to help keep the airway patent (open) & should not be used in the conscious patient with a gag reflex.
Now this is a bite block (image 2), which can be used for that patient biting on an E.T. tube.
 |
| Image 2 "Bite Block" |
Labels:
commentary
Friday, March 25, 2011
SmartCare "Too Short for This Ride"
 | ||||||||||||||
I remember when I was younger how upset I got over the fact that I was too short to ride a stand up roller coaster. It would have been not so traumatic; however my younger brother of two years was able to ride and antagonized me the rest of the day.
Yes, I was the Husky (short & chubby) kid and isolated from sports where height is an advantage.
Being too short for riding a roller coaster or playing basketball is a common occurrence, however what about being too short for a mode of mechanical ventilation?
Labels:
SmartCare
Monday, March 21, 2011
Intrinsic PEEP (PEEP i)
 | |||
| Assessment of PEEPi based on a end-expiratory occlusion. Maneuver is high-lighted. |
Intrinsic PEEP (PEEPi) is the difference between total PEEP and external PEEP, and provides information on the amount of dynamic hyper-inflation working on the respiratory system as well as the intra-thoracic organs.
PEEPi has the same adverse effects of PEEP regarding both hemodynamics, barotrauma, and volutrauma.
PEEPi affects patient triggering by creating a inspiratory threshold load to be over come by the patient during spontaneous breathing.
Monday, March 14, 2011
Anesthesia Machines: Bellows vs. Piston
Correspondence 2008.
Attached are three documents:
1. Article on gas consumption in bellow driving anesthesia machines, comparing both Draeger & GE, this is one of the main reasons Draeger switched to a piston (to conserve on fresh gas, allowing for minimal flow anesthesia < or = 1/4 liter total fresh gas flow).
2. Abstract comparing the Apollo (piston) & Aisys (bellows) in regards to the accuracy of tidal volume delivery, with the new technology the Aisys can also accurately deliver both large & small tidal volumes.
3. A letter I wrote to a customer on the limitations of the (Draeger's) Narkomed 2B (an older bellows machine) in regards to ventilating the morbidly obese patient.
Labels:
Anesthesia
Wednesday, March 2, 2011
The Not So Smart, “SmartCare”
SmartCare/PS® or SmartCare Pressure support (™ Draeger Medical, Telford, PA) is the only automated weaning ventilator mode in the United States that relies entirely on a rule-based expert system[1]. Sales specialists are quick to insist that the software upgrade will pay for itself, and decease intensive care unit, ventilator days.
Before considering such a large capital purchase expense, one should consider the following; "Is SmartCare quicker then in-place protocols?" PEEP restraints during spontaneous breathing trials, and high intrinsic diaphragmatic rates.
Before considering such a large capital purchase expense, one should consider the following; "Is SmartCare quicker then in-place protocols?" PEEP restraints during spontaneous breathing trials, and high intrinsic diaphragmatic rates.
Is it Quicker?
The term "automated" is a little misleading, since the practitioner first has to identify if the patient is even a candidate to perform spontaneous breathing trials.
After screening the patient the operator needs to change the mode to "Spontaneous", and make selections under the following categories; Body weight, Airway Type, Medical History, & Night Rest.
Entering patient data into these categories determine rules for the ventilator to follow, in regards to pressure support titration, respiratory rate limits, and end-tidal carbon dioxide limits (etCO2).
After initiating a SmartCare session (starting the mode), the ventilator adapts the level of pressure support[2] to maintain the patient in a "Zone of Respiratory Comfort"[3], slowly progressing to a spontaneous breathing trial (SBT) at the rule-based predetermined minimum pressure support[4].
The quickest a patient can transition and complete a spontaneous breathing trial from the initiation of SmartCare is one (1) hour and two (2) minutes. This is much slower then the many standard Respiratory Therapist Driven Weaning protocols I'm familiar with. The current SBT protocol at seven different hospitals I'm familiar with, the SBT trial time is thirty (30) minutes (this is for both surgical & medical patients).
So at these facilities with proactive weaning protocols, Smartcare would be unnecessary.
Positive Expiratory End-Pressure restraints
Another consideration with SmartCare is that it will not perform a SBT on PEEP settings ≥ 8 cmH2O. Some institutions will use higher PEEP during SBT's with the morbidly obese patients and patients that have trigger asynchronies, secondary to dynamic hyper-inflation.
High diaphragmatic frequencies
Many patients receiving mechanical ventilation have high intrinsic diaphragm rates (≥ 30), even when very well assisted. This usually is unnoticed because the ventilator only measures machine or patient triggered breaths; however the patient's true rate may be higher. The practitioner may notice ventilator flow distortions, in which the patient is attempting to initiate a breath however the machine doesn't provide one (a.k.a ineffective efforts, or missed trigger attempts).
This is a problem with the SmartCare classification models.
 |
| Missed Trigger Attempts, notice the flow distortions (purple flow waveform) without associated breaths. Measured rate 12 bpm, however intrinsic rate 30 bpm. |
This is a problem with the SmartCare classification models.
After pressure support is decreased and the patients true respiratory rate is unmasked (by the reduction in ineffective efforts) a patient who has a rate of ≥ 30 bpm with no other manifestations of distress, will never be classified "Normal Ventilation", they will be classified as "Tachypnea" or "Severe Tachypnea".
A seasoned Respiratory Therapist may notice that the patient is actually becoming more synchronous at the lower levels of support; the SmartCare model will fail the patient and increase the pressure support setting.
Dr. Magdy Younes stated in a lecture on ventilator synchrony[5], that in his sampled ventilator population that 50% of his ICU patients had a diaphragm rate > 30 bpm and 25% of these patients had a diaphragmatic rate > 35, even when very well assisted.
So, in this patient population SmartCare would be a poor choice for a weaning modality.
In my own ICU patients I sampled ~ 20 patients and I calculated that 7% had intrinsic diaphragmatic rates > 30, even in patients that the minute ventilation was 100% supported by the ventilator (e.g. 72kg IDW patient, preset minute ventilation of ≥ 7.2 liters).
Conclusion
SmartCare is an automated weaning platform which uses an intelligent control scheme to wean mechanically ventilated patients. Even though the system is automated the operator still needs to first determine if the patient is ready for SBT's and second select a few basic parameters before initiating the mode. In comparison to Respiratory Therapist Weaning protocols, SmartCare may be much slower in performing a SBT. In regards to higher PEEP levels and higher intrinsic diaphragmatic rates, SmartCare's models will not perform a spontaneous breathing trial in these patients.
[1] Chatburn, R. & Mireles, E. (2011). Closed-loop Control of Mechanical Ventilation: Description and Classification of Targeting Schemes. Respiratory Care. 1 (56).
[2] SmartCare continuously monitors EtCO2, Vt, & RR (measurements collected every 10 seconds). With these measurements the software classifies the patient status every 2-5 minutes. Based on the classification status the ventilator will ↑ or ↓ pressure support, or set-off an alarm condition.
[3] Zone of Respiratory Comfort is based on patients' weight selected & medical history.
[4] Minimum pressure support level is predetermined by Airway Type, active humidifier vs. heat moisture exchanger.
[5] Magdy Younes presented a lecture circa 2006, on ventilator asynchrony & PAV+ it was recorded for Covidien.
RELATED LINKS
New auto-weaning ventilator might make pulmonologist obsolete
RELATED LINKS
New auto-weaning ventilator might make pulmonologist obsolete
Labels:
SmartCare
Subscribe to:
Posts (Atom)

